Basic Kidney Anatomy
- Kidneys paired, about 150 gm each
- Urine forming units:
- Cortex
- Medulla (lobed: renal pyramids)
- Cortex and medulla composed chiefly of nephrons and blood vessels
- Supplied by renal arteries (branches of descending aorta) and renal veins (branches of inferior vena cava)
- Urine collecting and expelling units:
- Calyces
- Renal pelvises
- Ureters
- Bladder
- Urethra
Although the Kidneys are Tiny Organs They Receive 25% of the Cardiac Output
- The 2 kidneys are only 0.4% of the body weight but receive about 25% of the blood flow
- Blood flow rate per kilogram of tissue is almost 8 times higher in the kidneys than through muscles doing heavy exercise!
- Kidney: 4 liters/kg-min
- Exercising muscle: 0.55 liters/kg-min
- Blood flow rate per kilogram of tissue is almost 8 times higher in the kidneys than through muscles doing heavy exercise!
- Extremely important function: to regulate the composition and volume of body fluids
- Blood flows in and out of kidney leaving behind the 1% which becomes urine
- Urine flows through ureters to bladder and then through urethra to outside world
- The bladder is under both voluntary and autonomic control
Kidneys Filter About 180 Liters of Plasma Every Day, But Make Only 2 Liters of Urine
- The kidneys filter approximately 180 liters of plasma/day (each of the 3 liters of plasma gets filtered about 60 times)
- To replace this much water you would have to drink a 12 ounce soft drink every 3 minutes of the day
- Fortunately 99% of the filtrate gets reabsorbed, leaving 1.5-2 liters of urine per day
- It is remarkable that the kidney filter can be used continuously for 70 years or more without becoming clogged
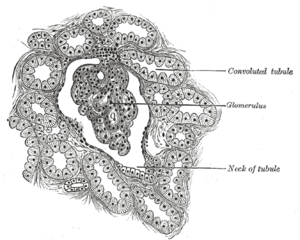
The Nephron is the Fundamental Urine-Producing Unit of the Kidney
- We have a total of 2 million nephrons in the 2 kidneys when we are young
- Components of the nephron (see diagram below):
- Glomerulus– tuft of capillaries where filtration occurs
- Bowman’s capsule– surrounds glomerulus, collects filtrate
- Proximal convoluted tubule
- Loop of Henle
- Distal convoluted tubule
- Collecting duct- adjusts volume & concentration of urine
- Distinctive feature: the tubule makes a sharp bend at the loop of Henle
- Because of the bend, tubule fluid moves downward into regions of increasing osmotic pressure (see diagram below)
- After the bend the tubule fluid moves upward through regions of decreasing osmotic pressure
- Glomerulus has large pores, allowing filtration of large volumes of fluid
- Number of nephrons declines with age, to about 50% at age 60; this causes the GFR to drop to 50% of value in a young person
- Loss of nephrons can cause drug overdose in older persons
The Basic Processes of the Kidney are Filtration, Reabsorption and Secretion
- Filtration:
- About 20% of the plasma that passes through the kidney gets filtered into the nephron
- Filtration is takes place in the glomerulus
- Driven by the hydrostatic pressure of the blood (osmosis opposes filtration, but the hydrostatic pressure is larger)
- Water and small molecules are filtered; blood cells and large molecules (most proteins) do not pass through the filter
- Reabsorption & secretion:
- As the filtrate passes down the nephron most of it is reabsorbed into the blood
| Substance | % Reabsorbed |
| Water | 99.4% |
| Na | 99.4% |
| K | 93.3% |
| HCO3 | 100% |
| Glucose | 100% |
| Urea | 53% |
| Inulin | 0% |
Data from: William Ganong. Review of Medical Physiology. 1999.
-
- A few substances are secreted from the blood to the nephron
- Reabsorption and secretion are energy intensive- the kidney is one of the most metabolically active organs in the body
- Filtering substances into the tubules and then reabsorbing nearly 100% of them, using energy, may seem to be a very wastefull process, but it allows the body to quickly remove many toxic substances from the blood (they are usually not reabsorbed)
- Net Process:
- Amt in Urine = Amt Filtered – Amt Reabsorbed + Amt Secreted
Glomerular Filtration is Easy to Measure From Inulin or Creatinine Clearance
- The rate at which the kidney filters blood plasma is called the glomerular filtration rate (GFR)
- It is relatively easy to measure the GFR and it is a good way of assessing kidney function
- Consider a substance, A, which is only filtered by the kidney; it is neither reabsorbed nor secreteted
- Since no A is reabsorbed from or secreted into the tubule, the amount filtered into the tubule at the glomerulus must equal the amount appearing in the urine
- P X GFR = U X V
- P = plasma concentration of A, in mg/mL
- GFR = glomerular filtration rate of plasma, in mL/min
- U = urine concentration of A, in mg/mL
- V = rate of urine production in, in mL/min
- Solving the equation for GFR will give:
- GFR = (U X V)/P
- Since no A is reabsorbed from or secreted into the tubule, the amount filtered into the tubule at the glomerulus must equal the amount appearing in the urine
- Two substances are used to measure GFR:
- Inulin: a polysaccharide which is not metabolized by the body. Inulin is not found in the body and must be injected. This substance gives the most accurate results and is used for research purposes.
- Creatinine: a breakdown product from creatine phosphate, which is naturally found in the blood. Not quite as accurate as inulin (about 10% is reabsorbed), but often used in medicine, since no injection is required.
- GFR measurements are very easy to do and give an assessment of kidney function. It is important to do these measurements in older patients and in others who may have kidney impairment
- For substances which are reabsorbed and/or secreted the formula is slightly different:
- P X C = U X V
- C = clearance rate of the substance (takes into account secretion and reabsorption)
- C = (U X V)/P
- Clearance measurements tell you how the kidney handles the substance:
- Filtered + reabsorbed: C will be less than the GFR
- Filtered only: C = GFR (about 120 mL/min)
- Filtered + secreted: C will be higher than the GFR
Tubular Reabsorption Has a Maximum Rate
- Most of the solutes filtered into the tubule are reabsorbed because they are too valuable to throw away
- In many cases reabsorption is by active transport, requiring ATP
- Because of the active transport the kidney is an energy intensive organ
- Example of active transport: Na, K pump:
- Most of the filtered Na is reabsorbed by the Na pump in the proximal tubule (~65%)
- Na pumping in the ascending loop of Henle sets of osmotic gradients that are used to regulate water (~25%)
- Fine tuning of Na is done by Na pumps in the distal tubule and collecting duct, which are controlled by the hormone, aldosterone
- Some reabsorption is by secondary active transport- the flows are indirectly coupled to the active transport of another substance (such as Na)
- Example of secondary active transport: Glucose reabsorption
- The proximal tubule has a mechanism for cotransport of Na & glucose
- The kidney can reabsorb glucose at a tubular maximum rate of 320 mg/min
- If plasma glucose is normal (about 100 mg/deciliter) 125 mg/min of glucose is filtered into the tubules
- At this filtration rate the kidney can reabsorb 100% of the glucose in the proximal tubule
- If the plasma concentration gets high enough (about 300 mg/deciliter) the filtered glucose rate will exceed the tubular maximum for glucose
- When that occurs, some glucose will be excreted into the urine (glucosuria)
- This is the cause of urinary glucose in diabetes mellitus
- Note: small amounts of glucose may spill into the urine when plasma concentrations are as low as 180 mg/deciliter. This occurs because some of the nephrons have lower tubular maximum rates than others
- Second example 2: Water reabsorption
- Due to osmosis, but the osmotic gradients are set up by Na active transport
- There are maximum rates (tubular maximums) for reabsorption by active transport or secondary active transport
- Maximum transport rate is limited by the number of pump or carrier molecules in the cell membrane
The Kidney is an Osmotic Machine
- Kidney uses active transport (especially of Na) to set up osmotic gradients
- Osmotic gradients are shown in the figure below: osmotic pressure in the cortex is isotonic (~300 milliosmoles/liter)
- As you move toward the medulla the osmotic pressure rises, to about 1200 milliosmoles/liter (hypertonic)
- A distinctive feature of the tubule is the sharp bend at the loop of Henle
- Because of the bend, tubule fluid moves downward into regions of increasing osmotic pressure (see diagram below)
- After the bend the tubule fluid moves upward through regions of decreasing osmotic pressure
- The kidney takes advantage of the osmotic pressure difference between tubule fluid and interstitial fluid to move water out of the tubule
- By changing the permeability of the collecting duct the kidney is able to make concentrated or dilute urine by osmosis

More Information
Johann Koeslag of the University of Stellenbosch, Tygersberg, South Africa, has a nicely illustrated internet essay, Kidney Physiology in a Nutshell.
If you develop a passion for the kidney (many physiologists do!) someday you will want to read this book on kidney evolution by Homer Smith:
- Homer Smith. From Fish to Philosopher. Boston: Little, Brown & Co., 1953.
Related articles by Zemanta
- Women with chronic kidney disease more likely than men to go undiagnosed (scienceblog.com)
- Heart Test Deemed OK Before Kidney Transplant (nlm.nih.gov)
- Failing heart, failing kidney: Double trouble? (scienceblog.com)

![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=f4848d53-345a-487f-b4a4-a97270255f14)